What we do
Monitoring & Feedback
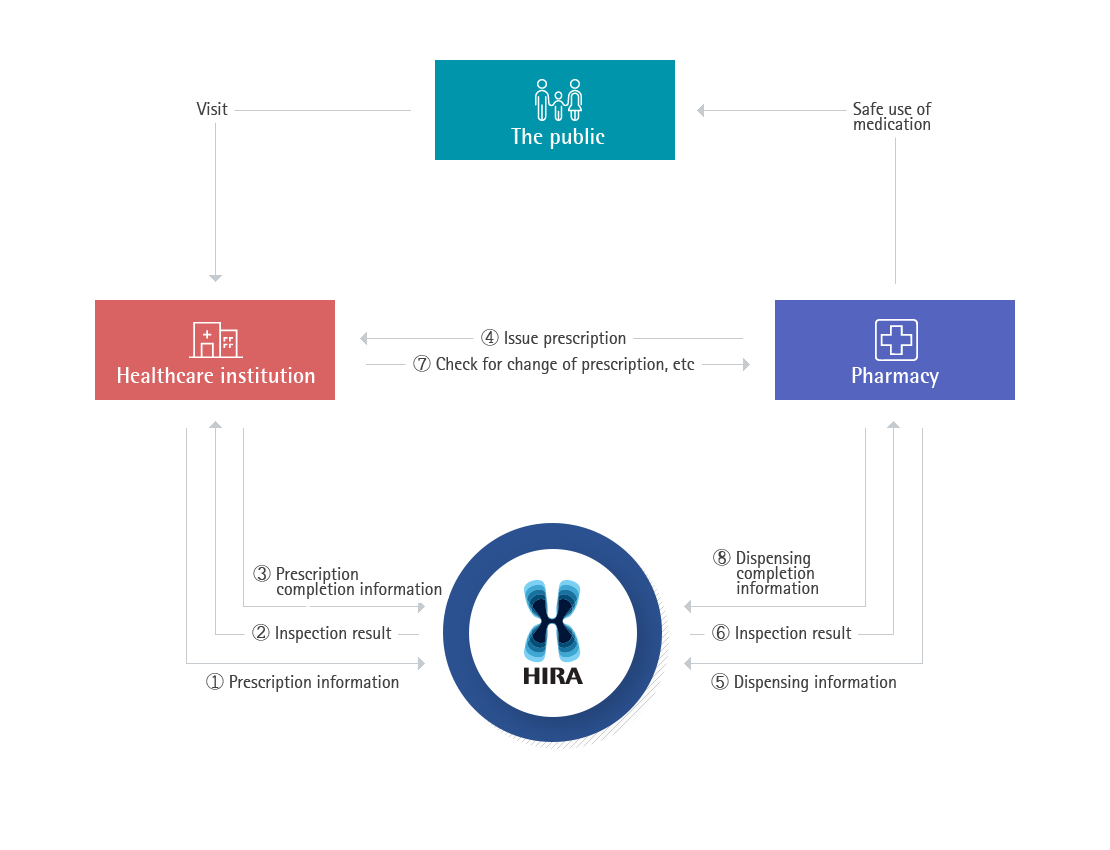
DUR Service procedure
- The doctor sends the details of prescription to HIRA DUR service before issuing the prescription to the patient. HIRA sends a warning message in a pop-up window on the doctors computer screen within 0.5 seconds, in case there is a risk factor in the prescription when compared to the patients medication history, suspended drug list, and DUR standards. The doctor could choose to change the prescription or to proceed with the original prescription with a memo, explaining why the drug should be used exceptionally. The final prescription information is sent to and stored in the DUR system of HIRA
- Pharmacists undergo the same process at the pharmacy when dispensing. For a warning message, the pharmacist could choose to change, or go ahead with the original prescription after checking with the doctor. The final dispensing detail information is sent to and stored in the DUR system of HIRA
Operational Performance
- The only system in the world which checks patients’ medication history on a real-time basis
- Prevention of drug misuse and abuse and reduction of pharmaceutical expenditure by preventing inappropriate use of drugs in advance (Saved over 20 billion KRW a year)
- Support safe prescription and dispensing practice by the real-time response (Prevented 5.4 million cases of unsafe use of drugs in prescription)
- Guaranteed fast response and 24/7 uninterrupted service
- A nationwide pharmaceutical monitoring system
- Support safe use of drug
- Facilitate links between computer systems via a standardized code
- Healthcare providers’ EMR and HIRA system are directly linked, expanding the information transmission channel
- Safe blood transfusion based on the patient medication history
- Based on the real-time drug monitoring, national level supervision is possible (epidemic, narcotic drugs, and etc.)
Medical claims portal service
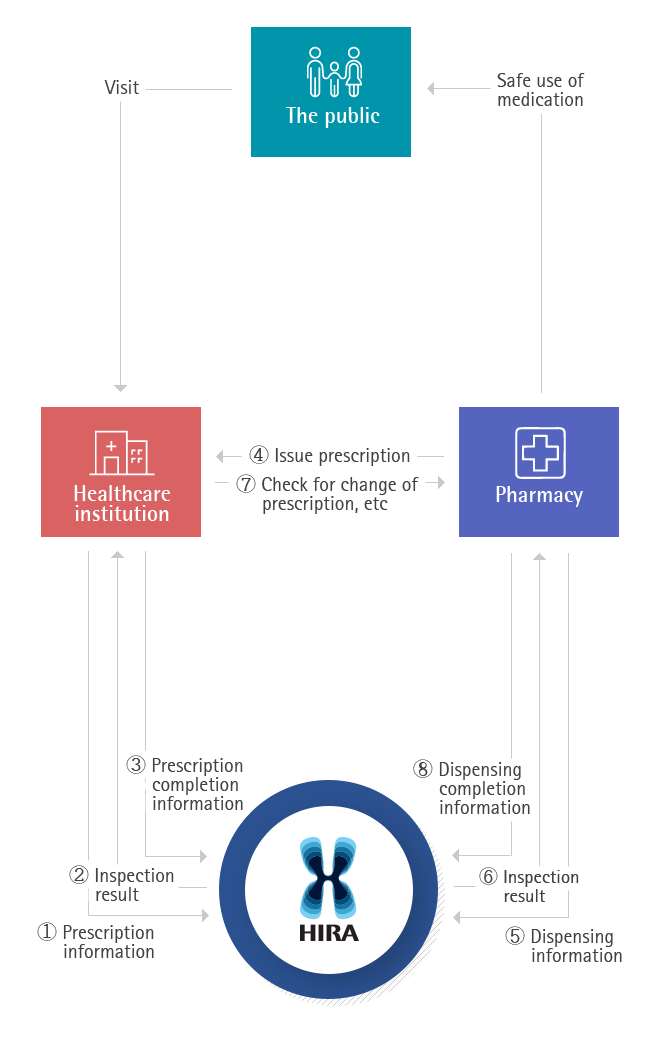
Benefit claim submission and result notice procedure
- Healthcare providers fill in benefit claim file using Claim Software accredited by HIRA. The file is inspected by benefit claim portal program before submission
- If the claim file passes the checkup process, it is compressed and encrypted to be sent directly to HIRA via the Internet with digital signature
- The claim file is verified by the digital signature, and transmitted to the review linkage system where the data set is decompressed, decrypted, and sent to the review system
- When the review is completed, a review result notification is produced, compressed, encrypted, and sent to the data center
- Healthcare providers receive and check the review result through the Benefit Claims Portal
Operational Performance
- Enhance national competitiveness by reducing social cost such as paper document resubmission costs, logistics costs, and etc (Replaced 1.4 billion paper documents with electronic documents in 2013)
- Support providers’ management efficiency by streamlining claims submission and reimbursement process (Claims review period : paper 40 days 구 electronic 15 days)
- Protect personal information and privacy by encrypting claims data
- Nationwide healthcare data supports policy-making process by collecting medical records swiftly and accurately
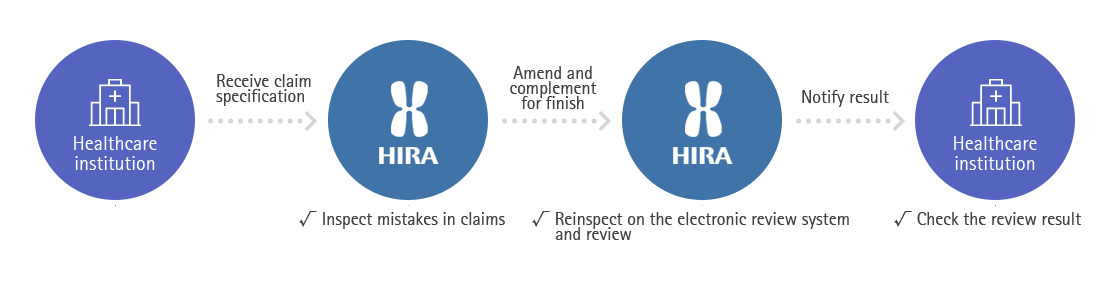
Medical claims review
Review procedure and types
- Claims review process starts with the submission of "benefit claim statement" by providers, which contains details of provided medical services and the cost
- [Electronic checkup] All statements go through electronic checkup to see the accuracy of basic information such as disease code, claim code, and the service price
- [Electronic review] By combining IT technology and review staffs knowhow, logical electronic review of six steps is conducted
- [Close Review] Claims that have high probability of error, or requires professional medical judgment are referred to review staff for a manual review. More complex cases are once again referred to committee member review, and to the review committee where experts gather to discuss the case
- [Post-management] For the cases that had unchecked items passed, HIRA operates post management of additional review to claw the misjudged benefits back. If providers or the insurer object to HIRA's decision, they can file an appeal with supporting materials.

Operational Performance
- Saving health insurance fund by preventing unnecessary expenditure
- Support providers’ administration efficiency by processing the review quickly
- Secure improved productivity, payroll cost reduction, and consistency in review result by utilizing Al
- Information management which enables real-time monitoring of review standard, review records, claim and review tendency
- Improve review quality by using knowledge utilized for review process (Review Knowledge Bank)
Quality assessment
Quality assessment procedure
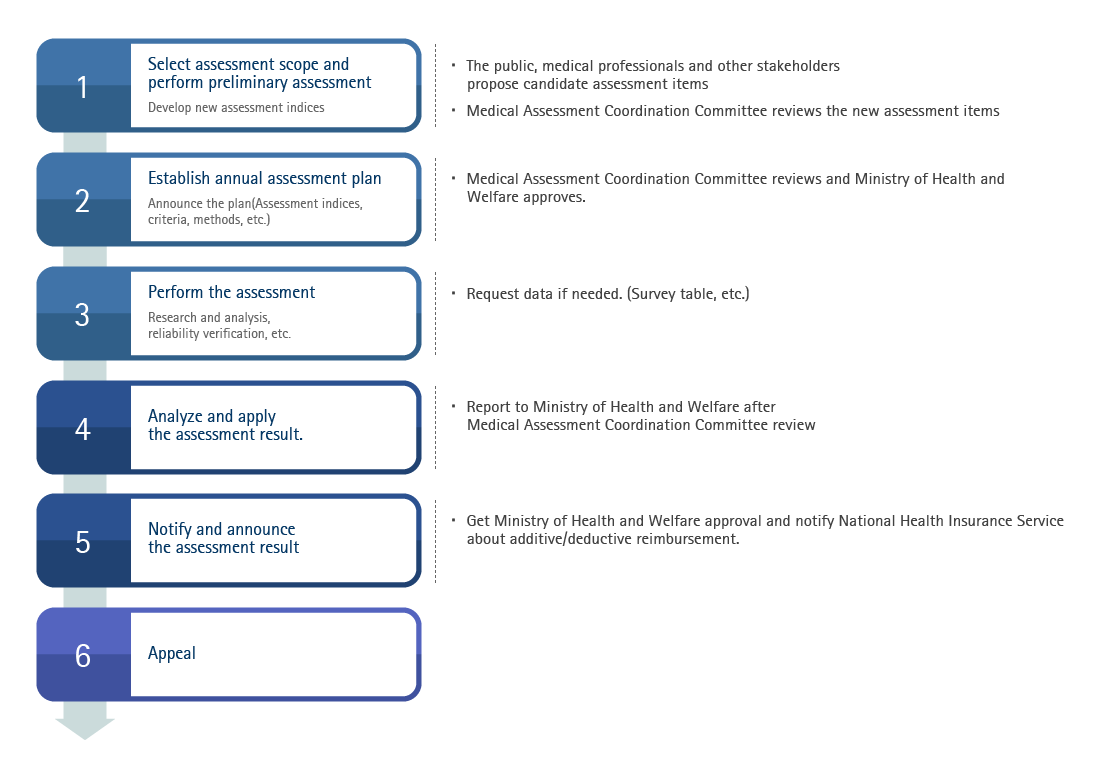
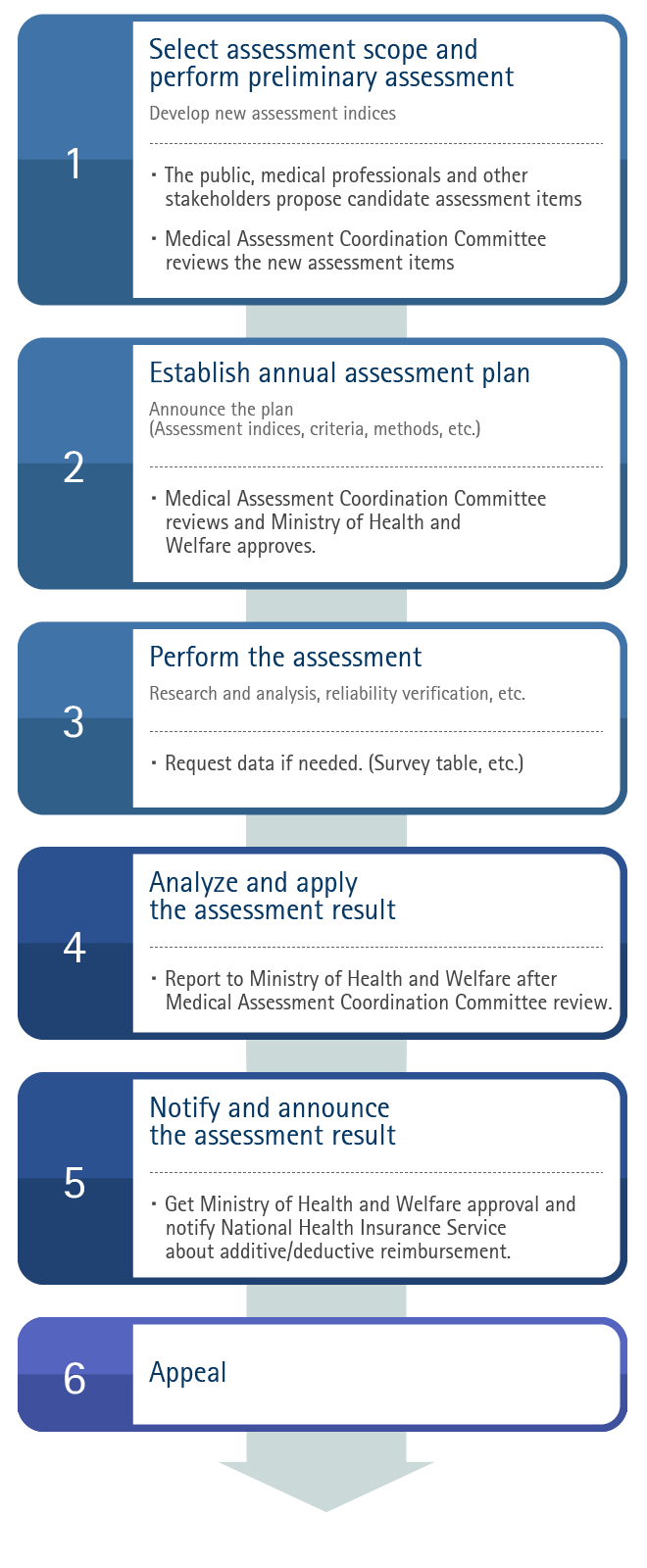
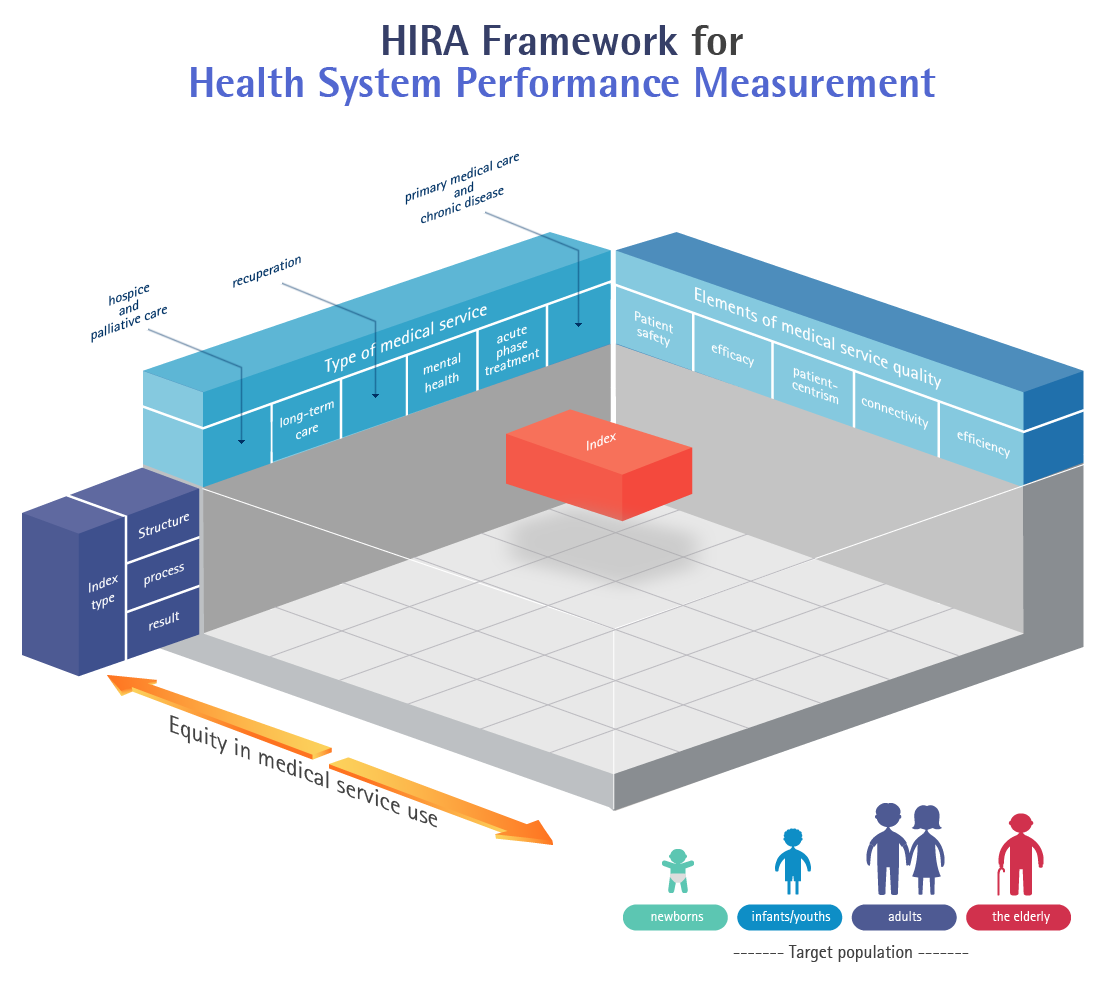
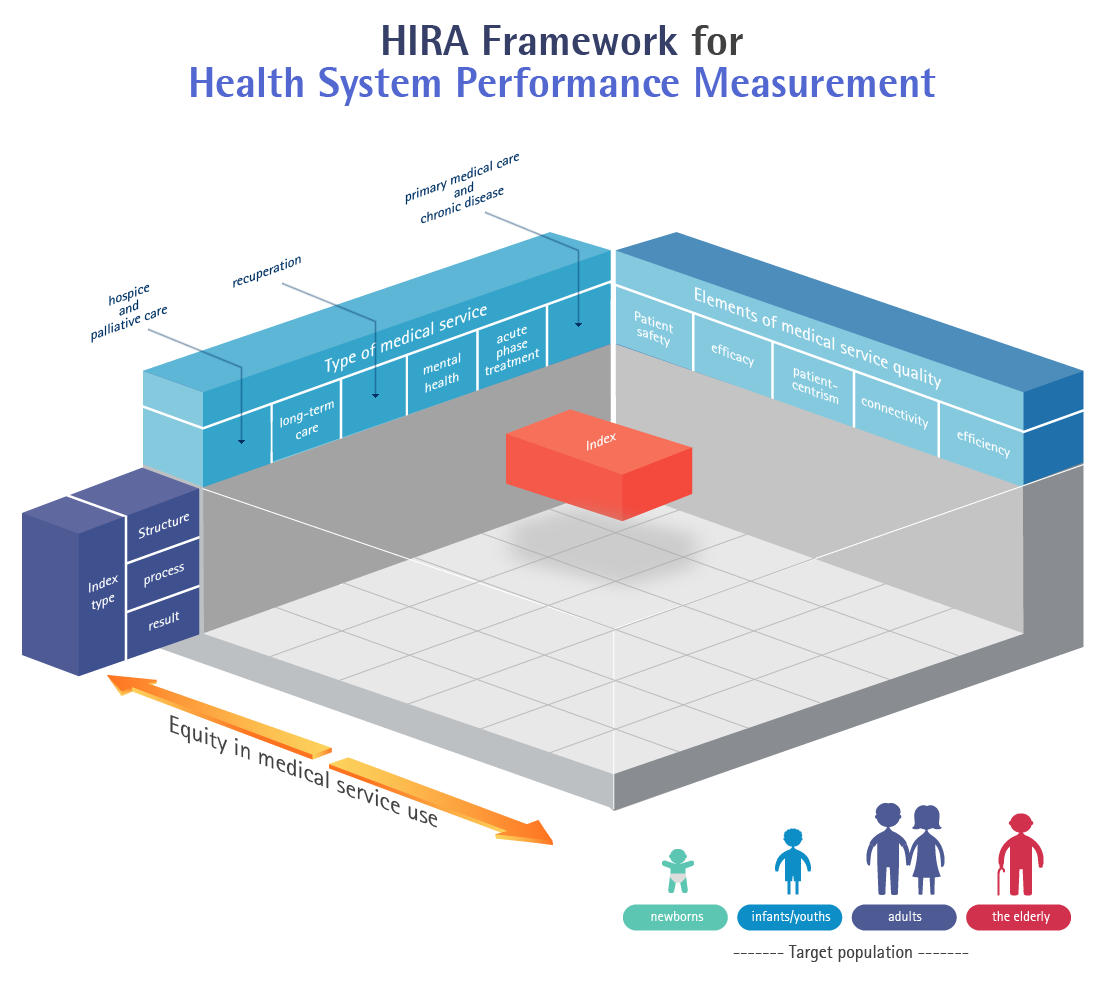
- Elements of medical service quality
| Type | Definition |
|---|---|
| Patient safety | Protect patients from possible danger during treatment. |
| Efficacy | Provide the best medical care to patients based on the most updated medical knowledge. |
| Patient-centrism | Provide medical care that fits the patient’s preferences, needs and values. |
| Connectivity | Coordinate and connect medical institutions and medical service types for the best treatment. |
| Efficiency | Maximize effect compared to used resources and minimize waste |
| Equity in medical service use | Provide equitable quality of medical care regardless of personal characteristics, including sex, age, region, and socio-economic status. |
- Type of medical service
| Type | Definition |
|---|---|
| Primary medical care and chronic disease control | The first type of medical service a patient experiences for treatment. It manages the patient’s health long-term, including chronic disease control. |
| Acute phase treatment | Medical service provided to patients in need of rapid treatment within a short period of time, including emergency, trauma, surgery, intensive care, in-hospital treatment. |
| Mental health | Prevention and early detection of mental disease and disorder. This service promotes counseling, treating, recuperating mentally ill patients and helps them return to the society, thereby improving quality of their lives. |
| Recuperation | Medical service that helps people with disability to lead their daily lives (kinesitherapy, language and occupational therapy, etc.). |
| Long-term care | Help patients who cannot take care of themselves to live safely and provide necessary nursing service. |
| Hospice and palliative care | Medical service aimed at providing comprehensive care and support in physical, mental, social and spiritual aspects to end-of-life stage patients and family. |
- Index type
| Type | Definition |
|---|---|
| Structure | Index evaluating whether manpower, facility and other structure are well prepared for providing good medical service. |
| Process | Index related to medical professionals activity through the whole process of providing medical service. |
| Result | Index related to the result of medical service, such as the usage of medical care, patient’s health as a result of medical service. |
Operational Performance
- Overall service quality improvement of all healthcare providers
Decrease the number of drugs per prescription(4.32 in 2002 → 3.64 in 2022), decrease the outpatient prescribed injection rate(38.62% in 2002 → 10.77% in 2022)
- Reasonable spending of health insurance fund by using assessment review results for Pay for Performance program
- Help the public choose healthcare provider reasonably, based on the assessment results
- Use the review result for the operation of healthcare system (selection of regional hub hospital, regional emergency medical center designation, comprehensive management of antibiotic resistance)
On-site Investigation procedure
- During the review and assessment procedure, HIRA may request an investigation of the providers who are likely to claim unfair charges. Also, Other institutions (Anti- Corruption & Civil Rights Commission, Public Prosecutors Office) may request an investigation of the providers who are likely to claim unfair charges or who have made unfair claims
- A reasonable investigation plan is established while considering urgency and efficiency. A recalculation process for adjustment is implemented with regard to payments made during the period subject to the investigation, based on the providers statement Based on the recalculation process, details of the appropriate course of administrative action are determined
- HIRA also announces the list of providers with unfair or illegal claims if they meet certain criteria.
- Post-management of the providers’ compliance of administrative measures such as service suspension is followed
Operational Performance
- Prevention of false claims and reduction of health insurance spending (Saving of about 20 billion KRW annually, indirect medical costs savings are very high)
- Create a healthy healthcare environment through investigation and monitoring for fraudulent medical activities
- Improve healthcare system (police effect) by investigating social issues (Increase in specific surgery numbers, excessive drug use, and etc.)
- Creating a healthy medical claims culture and preventing unnecessary healthcare spending
Medical fee verification procedure
- Patients may request HIRA to verify medical fee charged by providers for non cov-ered services are covered by National Health Insurance
- When patients request medical verification, HIRA may obtain related material from the provider and proceed with analysis and review (If necessary, Healthcare Review and Assessment Committee deliberation takes place). The results will be notified to the patient and provider
- The provider checks the result and refunds extra charge to the patient
Operational Performance
- Checks whether co-payment of non covered services were charged while complying with statutes (3 billion KRW reimbursement to patients annually)
- Protect the rights of patient by detecting false claims activities of providers
- Build trust process between providers and patients (provider - patient relationship)
